Plantar fasciitis
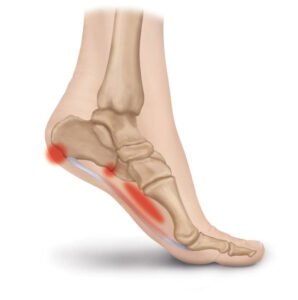 The plantar fascia is a strong, fibrous band of connective tissue that runs along the sole of the foot from the heel to the ball of the foot. Its role is to support the muscles of the foot, help maintain the arch and provide sensory feedback to the brain about foot and ankle position during standing and walking.
The plantar fascia is a strong, fibrous band of connective tissue that runs along the sole of the foot from the heel to the ball of the foot. Its role is to support the muscles of the foot, help maintain the arch and provide sensory feedback to the brain about foot and ankle position during standing and walking.
Plantar fasciitis occurs when this tissue becomes irritated or inflamed. Symptoms usually develop gradually, with pain often worst first thing in the morning or after periods of rest, and when weight bearing on the affected foot. Pain is typically felt in the sole of the foot towards the heel and can become sharp and limiting if the condition persists. If symptoms are not addressed early, plantar fasciitis may become more chronic, with changes in the collagen fibres of the fascia leading to reduced tissue resilience over time.
Causes of plantar fasciitis
Several factors can contribute to the development of plantar fasciitis, often in combination:
- Calf muscle tension – particularly where ankle flexibility is reduced
- Overuse – a sudden increase in walking, running or time spent on the feet
- Foot shape and arch type – both high arches and flat feet can increase strain on the plantar fascia
- Footwear – shoes with poor cushioning, minimal arch support or prolonged use of high heels
- Increased body weight – placing greater load through the foot
- Hip and buttock muscle weakness – particularly reduced strength in gluteus medius, which can alter pelvic and leg mechanics and increase load through the inside of the foot
- Direct trauma – such as landing on a hard or pointed surface
Treatment of plantar fasciitis
Osteopathic treatment involves assessing the whole biomechanical chain, from the foot upwards through the ankle, knee, hip and lower back, to identify contributing factors. Treatment is tailored to the individual and may include hands-on techniques to address muscle tension, joint restriction and movement patterns, alongside advice and exercises.
Self-management strategies commonly include:
- Stretching – particularly calf stretches, which can help reduce tension through the plantar fascia
- Plantar fascia self-massage – gently rolling the sole of the foot over a ball while seated, keeping pressure light initially
- Relative rest – reducing prolonged standing and high-impact activity during painful phases
- Activity modification – temporarily replacing running with lower-impact activities such as swimming or cycling
- Heat or cold – ice may be helpful in the early acute phase, with heat often better tolerated once symptoms settle
- Footwear and insoles – supportive shoes and appropriate insoles can reduce strain while symptoms are present
Plantar fasciitis can be slow to settle if ignored, but with appropriate assessment, treatment and guidance, symptoms often improve and function can be restored.
Appointments can be booked via my online diary.





